A Team Approach
In Olive Panning’s short life, she has undergone one complex medical procedure after another. Her medical conditions, fueled by a series of rare congenital issues, have kept her parents, physicians and caregivers on their toes for the last two-plus years.
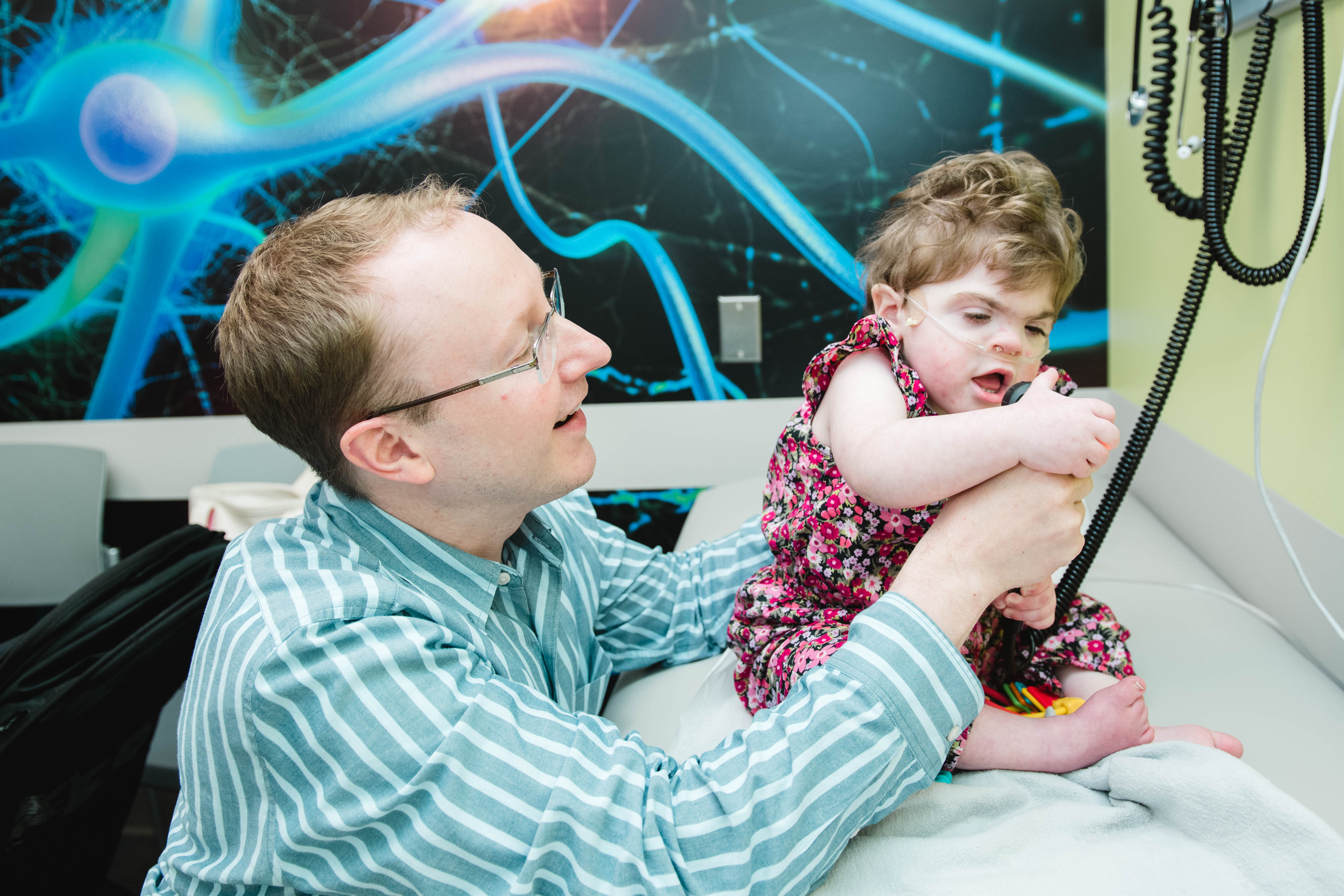
Beloved throughout Connecticut Children’s, where she currently sees 13 specialists, Olive, who is both legally deaf and blind, lights up every room she enters. And while her medical challenges have been many, she’s a fighter.
“Everything that has been thrown at her, she has powered through,” said Frederic Bernstein, DO, Director of Interventional Pediatric Cardiology and Olive’s primary cardiologist at Connecticut Children’s. “She’s had cardiac abnormalities on both sides of the heart, and she’s had multiple procedures and surgeries with us. She is definitely a ‘team-approach’ child because everything is interconnected,” he said.

Matters of the Heart—and Lungs
Before Olive was born, Adrienne and James Panning knew their baby had a heart defect. “We did a fetal echocardiogram, so we knew she had a cardiac issue,” Adrienne said. But the Simsbury couple were not expecting the myriad issues that followed their daughter’s birth on October 18, 2016.
Arriving just four days past her due date, Olive was delivered via Cesarean section, weighing 5 pounds, 12 ounces. Within 24 hours, she was transported to Connecticut Children’s Level 4 Neonatal Intensive Care Unit (NICU) for expert follow-up care.
“Pretty much right away she was diagnosed with pulmonary hypertension,” Adrienne said. Pulmonary hypertension is a rare, life-threatening type of high blood pressure that affects both the lungs and the heart. The right side of the heart works hard to pump blood through the lungs to pick up oxygen. Pulmonary hypertension makes the process harder to get blood through the lungs, therefore, creating a bottleneck getting blood to the left side of the heart, where it then leaves to go out to the body.
During cardiac catheterization, Olive’s Cardiology team found that her left pulmonary artery had split off and had “looped” around her esophagus, resulting in what’s known as a pulmonary sling. This rare condition causes compression of the trachea and esophagus and can lead to severe respiratory distress.
“She had respiratory issues on top of cardiac issues,” Adrienne said.
While her cardiac issues were being sorted out, Olive and her parents underwent genetics testing. Her mom and dad were surprised to learn that Olive has a rare chromosomal abnormality known as Unbalanced Translocation, a major contributor to neurodevelopmental disorders.
“It’s complicated,” Adrienne said, “but she has an extra part of Chromosome 4 and is missing part of Chromosome 18. We found out that my husband is a carrier.”
“We believe everything that is happening to Olive is due to her chromosome structure,” Adrienne said. Olive’s sister, Hattie, who was born in February 2019 does not have the chromosomal abnormality and is not a carrier.
After five weeks of hospitalization, first in the NICU and then in the Pediatric Intensive Care Unit (PICU), Adrienne said she and James decided to take their baby home, putting off the pulmonary artery sling repair until after the Thanksgiving holiday.

Olive and the “Blues”
Then in December, Olive began having frightening “blue spells” in which her lips, face and body would turn blue and she would lose consciousness.
Olive’s blue spells—or cyanosis—are a result of inadequate oxygen and circulation getting to certain areas of her body. For Olive, this is due to a combination of her pulmonary and cardiac issues.
The first time it happened, Adrienne was terrified. “I can’t recall why Olive started crying, but I noticed her lips turned blue and that’s when I realized she was holding her breath and not breathing. I pulled her out of her car seat, walked around with her and was jostling her—in a good way—to stimulate her. She eventually came to. At that time, she was not on oxygen, so I was probably more concerned about her ability to breathe again than I was a few months later.”
Adrienne and James learned that sometimes Olive would start crying and not take a breath quickly enough. Her lips would go blue, then her face and the rest of her body. She would lose consciousness and her whole body would become stiff. “We would try to stimulate her by rubbing her chest and blowing in her face until she takes a breath again,” Adrienne explained. “This is all maybe 10-20 seconds from blue lips to full color again and breathing.”
“It was the blue spells that were the deciding factor to get her heart surgery done right away,” Adrienne said.

Saving Olive
Olive’s heart surgery was scheduled for January 16, 2017, three months after she was born. “The surgery itself went well,” Adrienne said. It took place on a Monday morning, but the following night, Olive went into cardiac arrest.
“I will never forget that phone call,” Adrienne said. “It was 12:15 a.m. She coded and everything in my life changed. My husband and I were both asleep. We live in Simsbury, but we were in her room by 1 a.m. ‘What are we going to walk into?’ we wondered. We thought it was over. But she was doing OK!”
Adrienne credits PICU nurse Allison Wooten, RN, with saving her daughter’s life. “Olive was not looking right, and Alli did the CPR and called the code. She was on top of it and ready to go.”
Allison remembers that night well.
“I remember we were tight for staffing that night,” said Allison, who has worked at Connecticut Children’s for the past 15 years. “I was concerned about Olive and for her well-being. It didn’t look like she was doing well on her respiratory support.”
Since beginning her shift at 7 p.m., Allison kept a close watch over Olive. “Over the next couple of hours, she looked better,” she recalled. “But when I went back around 11 p.m., she didn’t look like she was breathing. Then the alarm started sounding. When she wasn’t responding, I immediately called for support and other nurses ran in and saw we were in dire need.”
Allison said they immediately began CPR procedures. “She didn’t have a heartbeat,” Allison said. “It was not a short resuscitation because she was sick and had just had surgery.”
When they had stabilized her, Allison called Olive’s parents. “If I were the parent, I would want someone to call me,” she said. “I called and said, ‘You really need to come in as soon as possible.’”
When Adrienne and James arrived, Allison met them at the door. “It’s very hard to meet a family under these circumstances,” she said, “but I wanted to be the one to talk to them about what had happened.”
Challenges and Successes
Over the past two-plus years, Olive has been hospitalized a number of times. She underwent a second cardiac surgery on May 21, 2018, and had a pacemaker placed three days later.
“From a heart perspective, Olive’s doing great,” Dr. Bernstein said. “It’s been more than a year since she came to the cath lab.” At that time, she underwent an angioplasty to improve the size of the vessel that had undergone surgery and to improve the flow of the blood out of the heart. “She hasn’t needed any other interventions or touch-ups since then,” he said.
In addition to being followed in Cardiology, Olive is also a patient in several other specialties including Gastroenterology, Orthopedics and Speech Therapy, among others.
In Speech Therapy, Olive meets every week with Sara Burnham, M.A., CCC-SLP, a speech and language pathologist at Connecticut Children’s. Sara first began working with Olive when she was transferred to Connecticut Children’s NICU.
“At that time, we worked with her on oral feeding,” Sara said. “She went home with a feeding tube from the NICU, and I followed up with her afterward. I worked with her again after her cardiac arrest.”
Since then, Sara and her team have been working with Olive on increasing her intake of fluids and solid foods. Currently, Olive gets her nutrition through her “G” tube or gastrostomy tube. The tube is inserted through the belly to bring nutrition directly to the stomach, ensuring that she gets the fluid and calories she needs.
“Mom is hopeful that Olive will be able to eat and drink more by mouth,” Sara explained. “So, we work on eating pureed fruits and vegetables. We also work with a sippy cup and a straw.”
Olive mostly drinks water, but she has been learning to chew a variety of the softer foods, like yogurt melts and peanut butter puffs. “We’ve really made some great progress,” Sara said.
“Olive is so much fun,” Sara added. “She can light up a room, and her laugh is so contagious. She definitely knows me and our routine.”

Exploratory Surgery
Olive is also seen in Neurosurgery, where she has follow-up appointments with Markus Bookland, MD, a Connecticut Children’s neurosurgeon.
After Thanksgiving in 2018, Adrienne said Olive underwent exploratory surgery with Dr. Bookland to find out if she had a tethered spinal cord. A tethered spinal cord limits the movement of the spinal cord within the spinal column. The resulting tension impairs blood flow to the nerves and can cause symptoms, such as spine deformities and difficulties walking.
A tethered spinal cord is usually treated surgically by “freeing” the cord. To do that, Dr. Bookland created a small opening in Olive’s back. “We were able to release the tethering on her spinal cord at the bottom of the spine,” he said.
“She did very well,” Dr. Bookland added. “She didn’t throw us any curve balls. She had a common variant; the filum was thicker than it should have been.”
The filum is a fibrous structure that extends from the cone-shaped end of the spinal cord, usually around the first or second lumbar vertebrae, to the coccyx--a small triangular bone at the base of the spinal column.
“I’m very happy with how she’s doing,” Dr. Bookland said. “She’s showing some spunk and pushes up with her legs. She has shown real improvement in her tone, primarily in her ankles.”
Dr. Bookland said they will continue to follow Olive in the Division for the next two to three years. “But I am very optimistic that Olive will not need any more neurosurgery,” he said.

Other Specialties
Olive’s conditions have led her to other services provided at Connecticut Children’s, including Palliative Care. “Palliative care is about quality of life,” Adrienne said. “It’s about ‘How do you maximize the quality of life, no matter how long it is?’”
“They help with care coordination, and it’s been so helpful,” Adrienne said. “When you’re talking about a child with so many congenital conditions, how do you manage all that? They’ve really stepped in and helped us figure that out.”
As with her regular follow-up visits to Cardiology, Olive is also seen regularly in the Division of Pulmonary Medicine—just not as much these days.
“Olive came to us primarily because of multiple episodes of hospitalizations, including fairly significant ‘blue spells,’” said Craig Lapin, MD, a Connecticut Children’s pulmonologist. “By the time we started to see her when she was just under a year of age, it was obvious she had chronic changes to her lungs.”
Olive was having difficulties with repeated pulmonary aspirations in which she would breathe secretions, such as mucus or saliva, into her airways. Aspiration can cause choking as well as serious infection in the lungs.
Dr. Lapin started Olive on positive-pressure breathing treatments and a recurrent antibiotic regimen to get her chronic infections under control. “Also, because of her chronic infection and inflammation, she was essentially on chronic oral steroids, and we had her on oxygen to decrease the risk of ‘blue spells’ from pulmonary hypertension,” he said.
Today, Dr. Lapin sees Olive less frequently than he did at first. “She’s come a long way from a breathing standpoint,” he said. “We have been able to wean her down from oral steroids and diuretics, and Mom will tell you that she is no longer admitted on a regular basis for respiratory issues. She does continue to have an oxygen requirement, but she’s much better than she was.”
Future Is Bright
Despite the challenges Olive has faced, Adrienne said things are looking up. “She’s doing more than we ever thought she’d be able to do: She’s pulling herself up and is standing. She’s not walking yet, but she is motivated. She may need a brace on her right leg long-term, but she just goes everywhere.”
Although legally blind, Olive still has some sight—about 20/80. “While her eyesight is not correctable, we’re hoping her hearing will get better,” said Adrienne, who serves on Connecticut Children’s Family Advisory Council, Patient Family Experience and Patient Safety & Quality Committees. “We’re hoping she will be a candidate for Cochlear implants.”
And maybe learn sign language as well.
“Olive’s a really smart kid,” Adrienne said. “She’s a problem-solver, and she’s very independent. She knows what she wants and goes for it.”
To support patient care at Connecticut Children’s, make a gift online or explore the many ways to give.
Latest Articles

New Primary Care Center at Connecticut Children’s Honors Nancy Law, MD

Ellie’s Story: How Supporting Connecticut Kids Changes Lives
